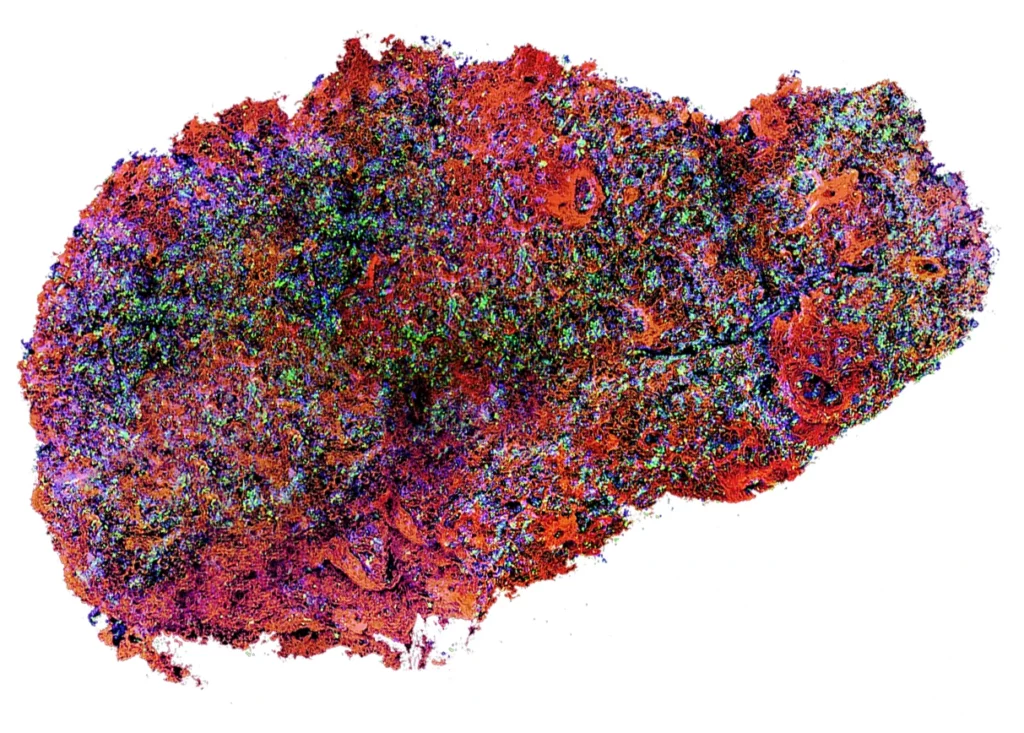
Our innovation combines state-of-the art stem cell technology with a breakthrough in tissue engineering to create a fully functional engineered micro-pancreas (EMP).
This has the potential to be a long-term solution for the management of diabetes, and to supply daily insulin replacement.
Our micro-organ matrix (MOM) recreates and mimics the normal extracellular environment that surrounds β-cells in the pancreas and supports their supply of necessary nutrients and growth factors.
About 500 million people worldwide are living with diabetes, a metabolic disorder caused by loss or dysfunction of beta(β)-cells in the pancreas and is associated with comorbidities and complications such as kidney and cardiovascular disease.
Currently, there is no long-term cure, and the only readily available treatment is replacement of insulin through injection, and careful control of sugar and carbohydrate intake to maintain blood sugar levels (glycaemia). There is a clear and urgent need to develop more advanced cell and/or regenerative therapies to restore normoglycemia in diabetic patients. Curing diabetes will require the restoration of β cell mass.
Transplantation of the insulin-producing unit of the pancreas, β-cell-containing islets, has been attempted in patients, with limited success: 70% of islets fail to engraft.
Importantly, isolated islets lack the molecular and structural microenvironment that is critical to their survival and function, and harvesting from cadaveric sources means high variability in quality and supply, making widespread adoption of the technique unfeasible.

Approaching regulators for First in Human studies

Viral clearance

Biocompatibility
A strategic decision taken to dedicate the resources to proceed development of MOM and outsource cell source to scalable stem cell derived beta cells
Devices for monitoring blood glucose and implantable insulin pumps are incapable of reproducing the fine-tuned glucose sensing of natural islets.
Patients still experience erratic swings in blood glucose, and dangerous episodes of severe hypoglycaemia. Islet cell transplant, introduced in 1999, is a more invasive procedure, requiring lifelong immune suppression;
70-90% of patients still need insulin injections within 5 years.
The supply of islet donors is extremely limited and variable, as the main source is from human cadavers, making this a non-scalable solution for the up to 5m people worldwide who need islet transplantation.
Cell-based regenerative therapies for the millions of people suffering from diabetes are therefore desperately needed.
Stem cell derived β-cells provide a more sustainable and successful source of material than islets.
“Naked” β-cells do not represent a long-term solution, however: most of the infused β-cells die after weeks.
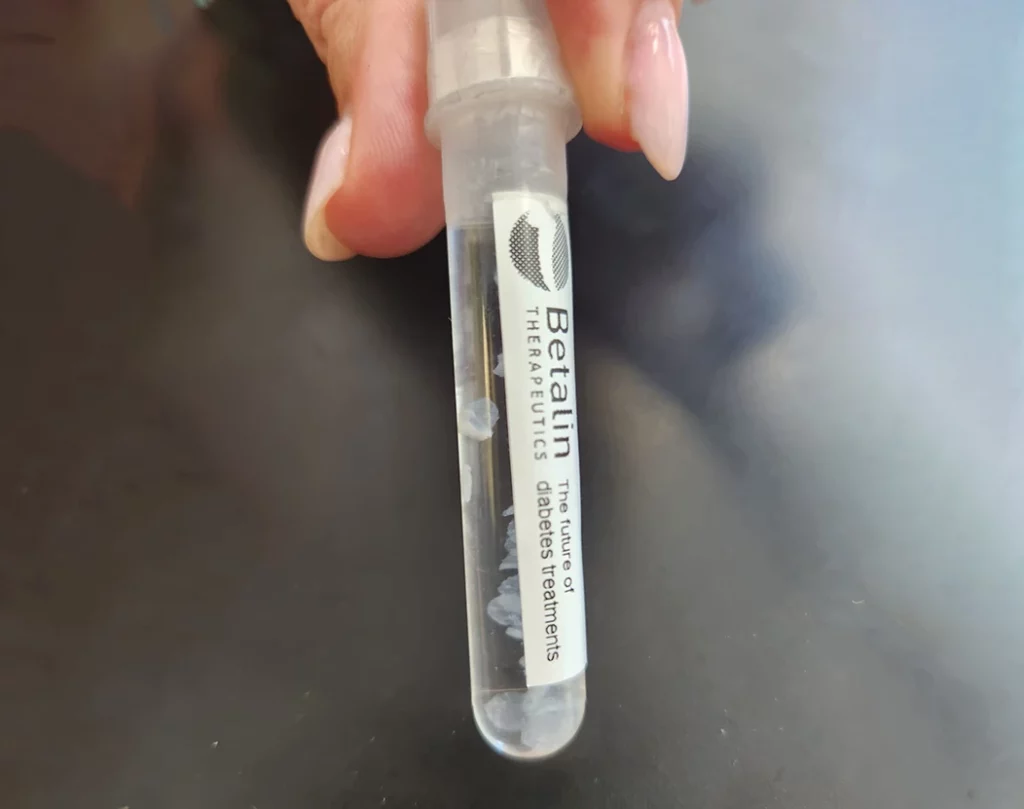
Unlike naked insulin producing cells that due to their small size (20 to 50 microns) migrate throughout the body, each micro-pancreas includes about 200,000 insulin producing cells and does not migrate.
The micro-pancreas technology, which applies scaffolds for cell support, leads to higher cell persistence and to significant increase of insulin production while reducing cell mortality.
The transplants will be more effective as the insulin secretion from the micro-pancreas is better regulated and insulin secretion from micro-pancreas lasts longer than the insulin secreted from cells alone.
Lowering the amount of insulin producing cells per transplant and higher success rates significantly reduces the transplantation costs.
With a commonly used device and under local anesthesia, the micro-pancreas is implanted subcutaneously into the patient’s abdominal or leg.
The micro-pancreas is delivered into the patient by subcutaneous implantation, enabling integration into recipient's tissues, without the need for risky surgery.
The micro-pancreas is suitable for outpatient clinics as the implementation does not demand expensive patient hospitalization.
Raised funds from private investors, the Israel Innovation Authroity and the Horizon 2020 Framework Programme of the Eurpean Union.

Betalin’s team is comprised of scientists, engineers, clinical experts, and a advisory board whose members include a Nobel prize winner and the President-Elect of the International Diabetes Federation.
The company is led by:










